Do you suffer dizziness? If so, you’re not alone. Symptoms of dizziness are amongst the most common symptoms we see in practice here at the Pinnacle Spine & Sports every day.
The question is, what causes it? And more importantly, WHAT CAN BE DONE ABOUT IT?
Dizziness is one of the most common presenting symptoms to clinical practice. It has been reported that 40-80% of neck traumatised patients experience vertigo, particularly following whiplash. The close relationship of the spine – particularly the neck with its rich sensory machinery – to postural control and balance means that the chiropractor is well placed to contribute to this large burden on the patient population. With so many possibilities, from simple functional impairments to serious life threatening emergencies it is important to be able to determine the cause of dizziness so that a prompt and calculated management plan can be applied to give the most likelihood of resolution.
A first consideration when dealing with a patient experiencing dizziness is to clarify the sensation experienced by the patient and to determine what the patient means when they state that they are “dizzy”.
The main considerations are:
- Do you feel light-headed as though you are about to faint, or is it more of a sensation of the world moving or spinning around you?
- How long does each attack of dizziness last?
- How long have you been experiencing these symptoms for, and have they been worsening over time?
- Do you also suffer tinnitus and/or hearing loss?
- Do you have any history of trauma to the head or neck?
A thorough history and a full physical & neurological examination will determine the cause of your dizziness. Common causes can include:
- Benign Paroxysmal Positional Vertigo (BPPV): This occurs when small crystals embedded within part of the vestibular apparatus become dislodged and make their way into the semicircular canals (where they shouldn’t be!) This effectively causes nerve signals from the vestibular apparatus to the brain to become amplified, and so movements of the head bring on an increased sensation of movement. The dizzy spell typically only last for 10-20 seconds, and is related to a positional change of the head (eg. rolling over in bed, looking down for a while then looking up, etc.) If the dizzy spell lasts any longer than 20 seconds it’s highly unlikely to be BPPV. If it is BPPV, a simple manoeuvre caled the Epley Manoeuvre can be carried out to correct it. In most cases, it only takes one or two applications of this techniaue to fix the problem.
- Meniere’s disease: This condition will be characterised by the classic triad of symptoms: vertigo, tinnitus (ringing in the ear), and hearing loss. The dizzy spells last longer in this condition, more like several minutes at a time.
- Infection (eg. acute otitis media or vestibular neuronitis): You’ve probably all heard of someone getting an inner ear infection, and the biggest effect is vertigo and a loss of balance. Again, dizzy spells last longer in the case of infection, and there is usually a history of a recent infection elsewhere in the body (commonly an upper respiratory tract infection).
- Acoustic neuroma: The 8th cranial nerve (the vestibulocochlear nerve) is the one that relays all vestibular signals AND sound information from the vestibular apparatus and the cochlea into the brain. This nerve is surrounded by a nerve sheath, and can become susceptible to the growth of a neuroma. This slow growing tumour will be responsible for the onset of dizziness and hearing loss over the course of years as it slowly compresses the nerve and inhibits nerve signals from travelling along it properly. It needs to be diagnosed by an MRI, and audiometry is frequently used to confirm the hearing loss prior to this (audiometry is also used when diagnosing Meniere’s disease).
- The main causes of vertigo that can be attributed to dysfunction of the brain or brainstem are:
- Multiple Sclerosis(MS): MS is definitely a consideration for vertigo sufferers, particularly if there have been episodes of dizziness in the past that have come and gone, or other neurological symptoms in the past that have seemingly spontaneously resolved themselves. It is also most common in caucasian or Mediterranean females aged between 20-50. MS attacks the myelin sheath that covers nerves and affects nerve transmission, showing up in a myriad of symptoms, of which attacks of vertigo can be one.
- Migraine: Yep, migraine. The more research we do into the brain the more we see that the neurological dysfunction that we classify as migraine is responsible for MANY different symptoms (not just headaches!) Headaches are just one of the many symptoms of migraine: vertigo is another. But that’s the topic of a whole separate blog entry.
- Vascular lesion: Damage to the vertebral artery (which supplies 30% of the blood to your brain) will lead to an alteration in the transmission of nerve signals and an alteration of perception of your position in space. This leads to dizziness as the brain isn’t exactly aware of the body’s location in relation to the environment around it. This also covers vascular lesions that have damaged the blood flow to the cerebellum, a part of the brain that is intricately involved in balance and co-ordination.
- Tumour: While rare, a space occupying lesion (ie. tumour) of the brainstem area must be considered as a potential causative factor in anyone with dizziness. This will usually correlate with a number of other history findings, and must be investigated with an MRI. Brainstem tumours are more common in children than in adults (adults tend to get tumours in higher areas of the brain, kids tend to get them in deeper areas of the brain such as the brainstem). Again, these are rare and anyone with dizziness SHOULD NOT assume they have a tumour! We’re not trying to scare anyone here…
Depending on the likely cause, we refer for further testing if necessary and liaise with your GP on your behalf. Once a diagnosis is made there are many ways that chiropractic treatment can help, especially if the cause is BPPV, migraine or if there is involvement of impaired sensory feedback from the cervical spine.
So what is dizziness?
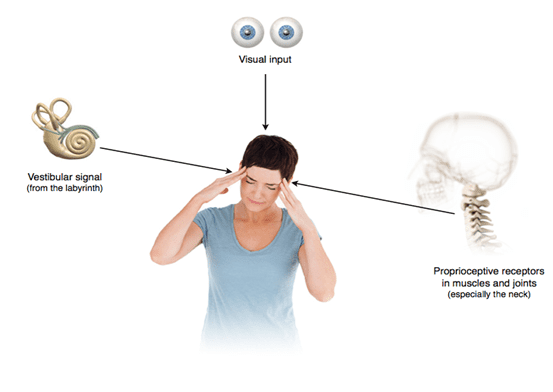
Dizziness is a non-specific term that describes a sensation of altered orientation in space. There are 3 major sensory systems involved in maintaining a clear perception of position and motion in space:
- Your eyes (visual inputs)
- The vestibular system (inner ear)
- Proprioception (or joint position sense, primarily from the upper part of the neck)
These 3 inputs converge onto the brainstem, and if all 3 are in agreement (ie. they’re all telling the brain the same thing regarding where the body is currently positioned in space), then a state of normality exists and there will be no sense of vertigo. If one of these 3 sensory inputs is a bit off, the brain can cancel that out and ignore it, and go with the other 2. If, however, there’s a mismatch between all 3 or a significant difference from one of them, a state of ‘unawareness’ ensues and the person will normally experience some vertigo.
Hence, improvement of the sensory information from the upper part of the neck (and rest of the body as a whole) with the aim of normalising these 3 sensory input systems will lead to a decrease in dizzy sensations. Isn’t it a good thing that chiropractic adjustments primarily enhance proprioceptive inputs into the brainstem?
This is one of the main ways that chiropractic can help with dizziness. Improving cervical (neck) proprioceptive feedback through adjustments to this area, will lead to an improvement in sensorimotor control and a greater sense of awareness of the body position in space, and any movement happening therein. A decrease in dizziness is commonly experienced through our treatment.


